Normally, urine contains chemicals that prevent crystals from forming. But what happens when you start to have pain in your back or side or you are having problems with urination? Could you be one of the thousands of people with kidney stones? The information below should give you a head start about this potentially serious health hazard.
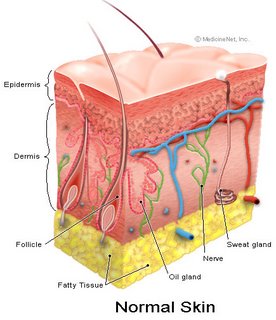
What happens under normal conditions?
The kidney performs many functions, the most important of which is the filtering of blood to remove toxins. Blood flows into the filtering component of the kidney called the glomerulus. The filtered portion of the blood then progresses through channels within the kidney, called tubules, which perform "fine tuning" of the filtering process. The final product of the filtered blood is urine, which gathers briefly in the renal pelvis and then is transported down the ureter, the muscular tube that carries urine to the bladder.
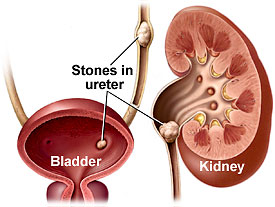
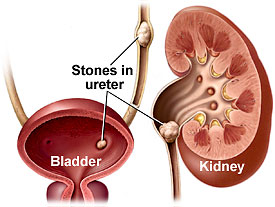
What are kidney stones?
Normally, urine contains many dissolved substances. At times, some materials may become concentrated in the urine and form solid crystals. These crystals can lead to the development of stones when materials continue to build up around them, much as a pearl is formed in an oyster.
The incidence of urolithiasis, or stone disease, is about 12 percent by age 70 for males and 5 percent for females in the United States. The debilitating effects of urolithiasis are quite substantial, with patients incurring billions of dollars in treatment costs each year. Stones occur more commonly in men than women, at a ratio of 3-to-1. In general, the peak incidence of stones occurs when a person is in their 30s.
The majority of stones contain calcium, with most being comprised of a material called calcium oxalate. Other types of stones include substances such as calcium phosphate, uric acid, cystine and struvite.
What are some risk factors for kidney stones?
A number of risk factors play major roles in stone formation. The first is loss of body fluids (dehydration). When one does not consume enough fluids during the day, the urine often becomes quite concentrated and darker. This increases the chance that crystals can form from materials within the urine, because there is less fluid available to dissolve them.
Diet can also affect the probability of stone formation. A high-protein diet can cause the acid content in the body to increase. This decreases the amount of urinary citrate, a "good" chemical that helps prevent stones. As a result, stones are more likely to form. A high-salt diet is another risk factor, as an increased amount of sodium passing into the urine can also pull calcium along with it. The net result is an increased calcium level in the urine, which increases the probability for stones. Intake of oxalate-rich foods such as leafy green vegetables, tea or chocolate may also worsen the situation.
Finally, a family history of stones, especially in a first-degree relative (parent or sibling), dramatically increases the probability of having stones.
What are the symptoms of kidney stones?
Once stones form in the urinary tract, they often grow with time and may change location within the kidney. Some stones may be washed out of the kidney by urine flow and end up trapped within the ureter. Stones usually begin causing symptoms when they block the outflow of the urine leading to the bladder.
Symptoms of an obstructing stone can vary. Most often, patients will complain of pain centered in their sides (flank), which may also radiate toward the front of the abdomen or to the groin area. At times, the pain may become so severe that the patient becomes unable to find a comfortable position. Blood in the urine (hematuria) may also appear when a stone is present. In some patients, especially those with diabetes, a fever may develop from infected urine that becomes trapped behind a stone. This is a medical emergency, as a bacterial infection that is not drained can cause a critical illness.
How are kidney stones diagnosed?
When a urinary stone is suspected, an immediate evaluation is required. Blood is obtained to check on overall kidney function as well as to exclude signs of infection throughout the body. Urine is sent for a urinalysis and culture. A simple X-ray of the abdomen is sometimes enough to pinpoint a calcification in the area of the kidneys or ureters, thus identifying a likely obstructing stone. If the X-ray film does not provide enough information to make a diagnosis, then an intravenous pyelogram (IVP) may be performed. A kidney blocked by a stone will not be able to excrete the dye from the IVP test as quickly and may appear enlarged. A final diagnostic exam that can be done is an abdominal/pelvic CT scan, which is very sensitive and can detect almost all types of urinary stones.
The abovementioned tests give your urologist information about the size, location and number of stones that are causing the symptoms. This allows the urologist to determine appropriate treatments.
How are kidney stones treated?
Stone size, the number of stones and their location are perhaps the most important factors in deciding the appropriate treatment for a patient with kidney stones. The composition of a stone, if known, can also affect the choice of treatments. Options for surgical treatment of stones include:
Shock Wave Lithotripsy (SWL): This is a completely non-invasive form of treatment in which an energy source generates a shock wave that is directed at a urinary stone within the kidney or ureter. Shock waves are transmitted to the patient either through a water bath, which the patient is placed in, or using a water-filled cushion that is placed against the skin. Ultrasound or fluoroscopy is used to locate the stone and focus the shock waves. The repeated force caused by the shock waves fragments the stone into small pieces.
SWL is most often performed under heavy sedation, although general anesthesia is sometimes used. Once the treatment is completed, the small stone particles then pass down the ureter and are eventually urinated away. In certain cases, a stent may need to be placed up the ureter just prior to SWL to assist in stone fragment passage.
Certain types of stone (cystine, calcium oxalate monohydrate) are resistant to SWL and usually require another treatment. In addition, larger stones (generally greater than 2.5 centimeters) may break into large pieces that can still block the kidney. Stones located in the lower portion of the kidney also have a decreased chance of passage.
Ureteroscopy (URS): This treatment involves the use of a very small, fiber-optic instrument called a ureteroscope, which allows access to stones in the ureter or kidney. The ureteroscope allows your urologist to directly visualize the stone by progressing up the ureter via the bladder. No incisions are necessary but general anesthesia is used.
Once the stone is seen through the ureteroscope, a small, basket-like device can be used to grasp smaller stones and remove them. If a stone is too large to remove, a laser, spark-generating probe or air-driven (pneumatic) probe can be passed through a channel built into the ureteroscope and the stone can be fragmented.
A straightforward case is complete once the stone has been shattered appropriately. However, if extensive manipulation was required to reach and/or treat the stone, your urologist may choose to place a stent within the ureter to allow the post-operative swelling to subside.
Percutaneous nephrolithotomy (PNL): PNL is the treatment of choice for large stones located within the kidney that will not be effectively treated with either SWL or URS. General anesthesia is required to perform a PNL. The main advantage of this approach compared to traditional open surgery is that only a small incision (about one centimeter) is required in the flank. The urologist then places a guide wire through the incision. The wire is inserted into the kidney under fluoroscopic guidance and directed down the ureter. A passage is then created around the wire using dilators to provide access into the kidney.
An instrument called a nephroscope is then passed into the kidney to visualize the stone. Fragmentation can then be done using an ultrasonic probe or a laser. Because the tract allows passage of larger instruments, your urologist can suction out or grasp the stone fragments as they are produced. This results in a higher clearance of stone fragments than with SWL or URS.
Once the procedure is complete, a tube is left in the flank to drain the kidney for several days.
Open surgery: A large incision is required in order to expose the kidney or portion of ureter that is involved with the stone. The portion of kidney overlying the stone or the ureteral wall is then surgically cut and the stone removed.
At present, open surgery is used only for very complicated cases of stone disease.
What can be expected after treatment for kidney stones?
Recovery times vary depending upon treatment, with the less invasive procedures allowing shorter recovery periods and quicker return to activity.
Shock Wave Lithotripsy (SWL): Patients generally go home the same day as the procedure and are able to resume a normal activity level in two to three days. Fluid intake is encouraged, as larger quantities of urine can help stone fragments to pass. Because the fragments need to pass spontaneously down the ureter, some flank pain can be anticipated. It is possible that the stone may not have shattered well enough to pass all of the fragments. If so, a repeat SWL treatment or other option may be required. If a stent was placed prior to SWL, this will need to be removed in your urologist's office within a few weeks. Stents are usually well tolerated by patients but can occasionally cause some bladder irritation and frequent urination.
Ureteroscopy (URS): Patients normally go home the same day and can resume normal activity in two to three days. As with SWL, if your urologist places a stent, it will need to be removed in approximately one week.
Percutaneous nephrolithotomy (PNL): After PNL, patients usually spend two to three days in the hospital. Your urologist may choose to have additional X-rays done while you are still in the hospital to determine if any stone fragments are still present. If some remain, your urologist may want to look back into the kidney with a nephroscope to remove them. This secondary procedure usually can be done with sedation and through the existing tract into the kidney. Once the stones have been removed, the stent coming out of the flank is removed and the patient can be discharged. Normal activity can be resumed after approximately one to two weeks.
Open surgery: Because these procedures are the most invasive and painful, patients often spend up to five to seven days in the hospital. Full recovery may take up to six weeks.
Postoperatively, your urologist will encourage a high fluid intake, to keep the daily volume of urine produced greater than two liters a day. In addition, you may need to undergo additional blood and urine tests to determine specific risk factors for stone formation and help minimize the chance for future stones. Although stone recurrence rates differ with each individual, a good estimate to keep in mind is a 50 percent chance of redeveloping a stone within a five-year period.
Frequently Asked Questions:
What are the risks or potential complications of the various treatments?
Each treatment has its own inherent risks. Some risks that can be associated with all surgical procedures are the possibility of bleeding and infection. It is extremely rare for patients undergoing shock wave lithotripsy (SWL) or ureteroscopy (URS) to have any problems with blood loss or infection. The probability is higher with more invasive treatments such as percutaneous nephrolithotomy (PNL) or open surgery. In most cases, patients do not require transfusion unless the procedure is unusually difficult.
With SWL, except in emergencies, patients must avoid aspirin, non-steroidal anti-inflammatory drugs such as ibuprofen or other blood thinners, as these can cause significant bleeding around the kidney. It is important that these medications be stopped at least one week prior to treatment if possible. SWL is generally a very safe treatment. Long-term follow up of patients has shown a slight increase in blood pressure, but no lasting adverse effect on kidney function has been noted.
In URS, there is a small possibility that the ureteral wall could be damaged or torn during the procedure. If this occurs, placement of a stent for two to three weeks is usually sufficient to allow the damaged area to heal. A complete tear of the ureter is very rare and requires open surgery to repair.
When PNL is performed, there is a small chance of air or fluids forming around a lung if the access channel is made toward the upper portion of the kidney. These entities are treated with a chest tube, which allows drainage of the fluid from around the lung. Other rare complications include injury to the bowel and injury to blood vessels within the kidney.
Will I have significant pain after the procedure?
Some discomfort is inevitable after surgical intervention for stones. The degree of discomfort is directly related to the invasiveness of the procedure. If needed, your urologist will prescribe medication to help control the pain during the recovery period.
What are signs of a problem postoperatively?
It is not uncommon for a patient to have a low-grade fever for the first 48 hours after surgery. However, if the fever continues or rises above 101.5° F (38.5° C) it could be a sign of active infection and should be reported to your urologist. Flank discomfort is also common after surgical interventions. However, if the pain becomes increasingly worse or unbearable, despite medication, your urologist should be notified.
How many times will I need to be treated?
The answer to this question depends on the size of stone and the treatment used. The chances for re-treatment are highest after SWL if the stone is large, extremely hard or in the lower portion of the kidney. PNL and open surgery tend to produce the highest stone-free rates.